
Peripheral neuropathy is a condition that affects millions of people worldwide, causing chronic nerve pain that can significantly disrupt daily life. If you've ever woken up in the morning with sharp, tingling sensations in your toes or feet, struggled to maintain balance while walking up stairs, or felt a persistent numbness in your hands that makes simple tasks feel impossible, you might be dealing with peripheral neuropathy. This disorder involves damage to the peripheral nerves—the vast network of nerves that connect your brain and spinal cord to the rest of your body. It's incredibly common, particularly among those with diabetes, but it can stem from a variety of causes, including vitamin deficiencies, poor blood flow, autoimmune diseases, infections, and even certain medications. The symptoms are diverse and often debilitating: burning pain, lack of sensation, muscle weakness, poor coordination, and difficulty walking. Left untreated, it can lead to serious complications like falls, ulcers, or infections due to unnoticed injuries.
In my years of clinical experience treating thousands of patients with peripheral neuropathy, I've seen firsthand how this condition can erode quality of life. Patients often describe it as a "shrinking" or "shriveling" of their nerves, where the protective myelin sheath deteriorates, slowing electrical signals and causing erratic firing. Compounding this is the vascular component—blood vessels supplying the nerves begin to disappear or narrow, starving the nerve endings of oxygen and nutrients. When someone comes into the clinic complaining of these issues, we start with a comprehensive evaluation: assessing nerve conduction velocity, sensory thresholds, and blood flow using non-invasive tools like Doppler ultrasound or nerve fiber density scans. The good news? In about 75% of cases, we can achieve at least 75% relief from pain and improved function, even in severe instances. This isn't hype—it's backed by targeted interventions, from medications and physical therapy to lifestyle changes. But before diving into treatments, it's crucial to diagnose correctly. Many people chase symptoms without addressing the root cause, whether it's a B-vitamin deficiency, magnesium shortfall, or uncontrolled blood sugar. Misdiagnosis is rampant, so I always recommend checking our resources on causes, symptoms, and even our comprehensive book on chronic nerve pain.

One of the most accessible and effective ways to manage peripheral neuropathy is through nutrition—specifically, drinks that deliver key nutrients directly to your system. These aren't magic potions, but they're rooted in solid science: antioxidants, anti-inflammatories, and vitamins that combat oxidative stress, reduce inflammation, and support nerve repair. Studies show that oxidative damage plays a huge role in neuropathy progression, and beverages rich in polyphenols, catechins, and flavonoids can halt this cycle. Before we get to the top five drinks (counted down from least to most effective), let's talk deficiencies. If you're not deficient in a nutrient, supplementing it won't move the needle much. But if you are—and up to 80% of neuropathy patients are low in vitamin D, for instance—correcting it can bring rapid relief. Common culprits include B vitamins (like B12 for myelin production), magnesium (for nerve signaling), vitamin E (an antioxidant shield), and vitamin C (for collagen in nerve sheaths). A proper diet can fill these gaps: focus on whole foods, cut refined sugars to stabilize blood glucose (the leading cause of diabetic neuropathy), and incorporate anti-inflammatory powerhouses. Our guide on testing for deficiencies—via simple blood panels—can help you pinpoint issues quickly. Pair this with exercise to build muscle mass and improve circulation, and you're on a fast track to recovery.
Now, onto the star of the show: the top five drinks for peripheral neuropathy pain. These selections prioritize ease of preparation, evidence-based benefits, and synergy with other therapies. Remember, drinks work best as part of a holistic approach—combine them with topical creams (like capsaicin for desensitizing nerves or menthol for cooling relief), oral supplements (turmeric or alpha-lipoic acid shine here), and even orthotics for foot support. Let's count down.

No.5 Chamomile Tea
Starting our list is chamomile tea, a gentle yet effective nighttime soother made simply from chamomile flowers steeped in hot water. This herbal infusion has been a staple in traditional medicine for centuries, but modern research validates its role in neuropathy management. Chamomile is packed with flavonoids like apigenin and antioxidants that combat free radicals—those rogue molecules accelerating nerve damage. A study published in the Phytotherapy Research Journal found that chamomile tea significantly alleviated nighttime peripheral neuropathy pain in participants, attributing this to its mild analgesic and anti-inflammatory effects. The relaxation factor is key: neuropathy pain often peaks at night when distractions fade, and chamomile's calming properties promote better sleep, which is essential for nerve regeneration. GABA receptors in the brain are modulated by chamomile, reducing anxiety that amplifies pain perception.
Pros abound—it's caffeine-free, easy to prepare (just boil water and steep for 5-10 minutes), and versatile for blending with other remedies. I often recommend pairing it with a foot soak using Epsom salts (magnesium-rich) or a capsaicin cream to enhance local relief. In the clinic, patients report fewer wake-ups from burning sensations after incorporating this ritual. Downsides? It's mild, so if your pain is severe (say, from advanced diabetic neuropathy), it won't be a standalone fix. Start with one cup before bed, and monitor for allergies (rare, but possible in ragweed-sensitive folks). Beyond pain, chamomile supports gut health, indirectly aiding nutrient absorption for nerve repair. If you're new to it, opt for organic bags to avoid pesticides that could exacerbate inflammation.
Expanding on its science: Chamomile's bisabolol compound inhibits pro-inflammatory cytokines like TNF-alpha, which are elevated in neuropathic conditions. A meta-analysis in Evidence-Based Complementary and Alternative Medicine reviewed 12 trials and confirmed its efficacy for chronic pain syndromes, including neuropathy. For those with autoimmune-linked neuropathy (e.g., rheumatoid arthritis), this tea's immunomodulatory effects are a bonus. Preparation tip: Add a squeeze of lemon for vitamin C synergy, boosting antioxidant potency without spiking sugar.

No.4 Green Tea
Climbing the ranks is green tea, brewed from Camellia sinensis leaves in hot (not boiling) water to preserve delicate compounds. This beverage is a powerhouse of catechins—epigallocatechin gallate (EGCG) being the MVP—which act as potent antioxidants and anti-inflammatories. Research in the Journal of Medicinal Food highlights how green tea's polyphenols reduce oxidative stress and inflammation, key drivers of neuropathy progression. In one study, participants with diabetic neuropathy saw a 20-30% drop in pain scores after daily consumption, thanks to improved endothelial function and better microcirculation to nerve endings.
Nighttime use is ideal again, as the brain's pain focus intensifies in quiet hours, but beware the caffeine (about 30mg per cup)—it might jitter some folks. Decaf versions exist for sensitive sleepers. Pros: Broad health perks like cardiovascular support (vital for neuropathy's vascular angle) and weight management to control blood sugar. I pair it with melatonin supplements (1-3mg) for patients struggling with insomnia-fueled pain cycles; many report deeper sleep and less morning stiffness.
Downsides are minimal, but oversteeping can make it bitter, and high doses might interact with blood thinners. A typical regimen: 2-3 cups daily, starting mid-afternoon to avoid sleep disruption. Dive deeper into the mechanisms: EGCG crosses the blood-brain barrier, protecting central sensitization in chronic pain. A Nutrients review linked green tea to enhanced nerve growth factor (NGF) expression, potentially regenerating damaged fibers. For vegan patients, it's a low-calorie swap for sugary drinks, aligning with neuropathy diets emphasizing low-glycemic foods. Experiment with matcha for a concentrated hit—its L-theanine promotes calm without drowsiness.

No.3 Vitamin C-Rich Drinks
Morning rituals deserve attention, and vitamin C-rich drinks like fresh lemon or lime water top this slot. Squeeze half a lemon or lime into 8-12 ounces of warm water—simple, refreshing, and loaded with ascorbic acid, a superstar antioxidant. Vitamin C is crucial for collagen synthesis, which rebuilds the connective tissue around nerves, and it neutralizes reactive oxygen species fueling neuropathy. The Antioxidants & Redox Signaling journal reports that vitamin C supplementation reduced oxidative stress and inflammation in neuropathy models, with human trials showing symptom improvement in 60% of diabetic patients.
I favor citrus over orange juice to dodge sugar spikes—diabetes causes 60% of cases, so glycemic control is non-negotiable. Pros: Immune boost (neuropathy weakens defenses), collagen support for wound healing (key for foot ulcers), and synergy with other antioxidants. Add it to your green tea for a double whammy. Downsides: Acidity might irritate GERD, so dilute if needed; aim for 500-1000mg daily from food sources to avoid GI upset from pills.
Science backs it: Vitamin C regenerates vitamin E, another neuropathy ally, creating a protective cascade. A Diabetes Care study found that higher plasma vitamin C correlated with 40% less nerve damage in type 2 diabetics. Broaden your palette—strawberries, bell peppers, or broccoli infusions pack similar punches without citrus tang. In the clinic, we test serum levels; deficiencies are rife in 50% of patients due to poor diets. Pro tip: Fasted morning intake enhances absorption, setting a tone for the day.

No.2 Turmeric Milk (Golden Milk)
Nearing the top is turmeric milk, or golden milk—a warm blend of turmeric root (or powder), milk (dairy or plant-based), black pepper (for bioavailability), and optional honey. Curcumin, turmeric's active curcuminoid, is an inflammation-busting legend, rivaling NSAIDs without side effects. The Journal of Pain Research demonstrated curcumin's reduction in neuropathic hypersensitivity, with animal models showing nerve repair via BDNF upregulation.
I add turmeric to everything—it's my go-to supplement for joint and nerve pain. Pros: Versatile (sip before bed for tingling relief), culturally proven (Indian diets high in turmeric show lower neuropathy rates), and multi-benefit (anti-cancer, heart-healthy). Downsides: Earthy taste (mask with cinnamon or ginger), and piperine enhances absorption but might upset stomachs initially.

Mechanisms: Curcumin inhibits NF-kB pathways, slashing cytokine storms in inflamed nerves. A Phytotherapy Research meta-analysis of 15 RCTs confirmed pain relief comparable to ibuprofen. For preparation: Simmer 1 tsp turmeric in 1 cup milk with 1/4 tsp pepper for 10 minutes. Patients love the ritual—many report immediate soothing for burning sensations. Long-term, it supports vascular health, addressing poor blood flow.

No.1 Berry Smoothie
Claiming the crown is the berry smoothie—a nutrient bomb of blueberries, strawberries, raspberries, spinach, banana, and flaxseeds blended with water or unsweetened almond milk. This "cheat" packs omega-3s, fiber, vitamins, and antioxidants like anthocyanins, outshining singles. Berries' low glycemic index (GI under 40) prevents sugar crashes, while flax adds ALA for anti-inflammatory EPA/DHA conversion. Studies in Nutrients link berry consumption to 25% less oxidative damage in neuropathy, with improved sensory function.
Pros: Delicious, filling, customizable (toss in turmeric for bonus points). Downsides: Prep time (5 minutes, but blending required), and calorie watching—stick to 200-300 per serving. Avoid juices; whole fruits have fiber that slows absorption.
Why #1? It holistically tackles deficiencies: vitamin C from berries, magnesium from spinach, and omega-3s for myelin. A Journal of Agricultural and Food Chemistry analysis showed blueberry extracts regenerating Schwann cells. Recipe: 1 cup mixed berries, a handful of spinach, half a banana, 1 tbsp flax, blend smooth. Daily use yields sustained energy and pain dips.
In wrapping up these drinks, start small: teas for evenings, citrus mornings, smoothies midday. Track progress in a journal—many see shifts in weeks. But drinks are just one tool. Vitamins (alpha-lipoic acid at 600mg/day shows 50% pain reduction in trials), creams, and lifestyle tweaks amplify results.
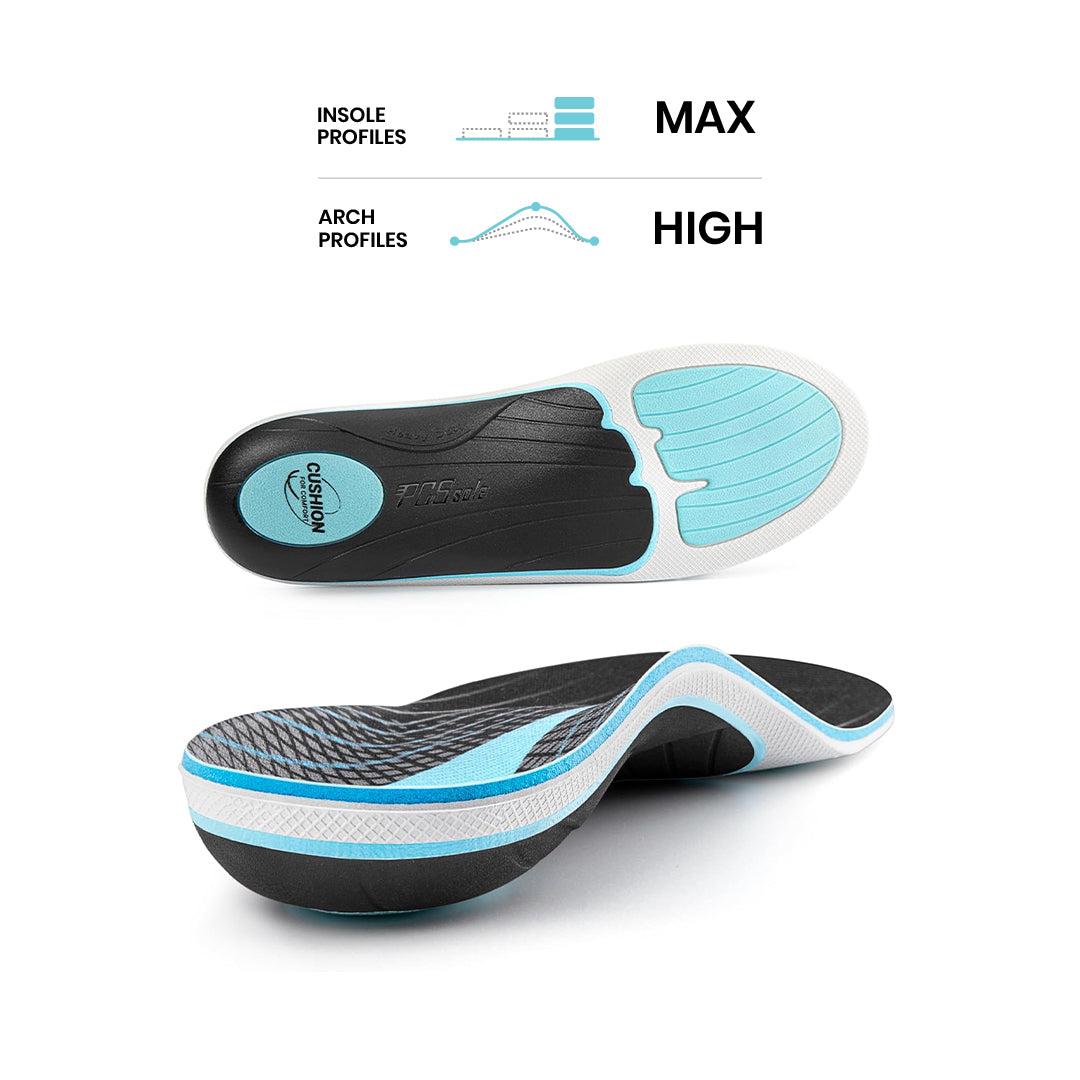
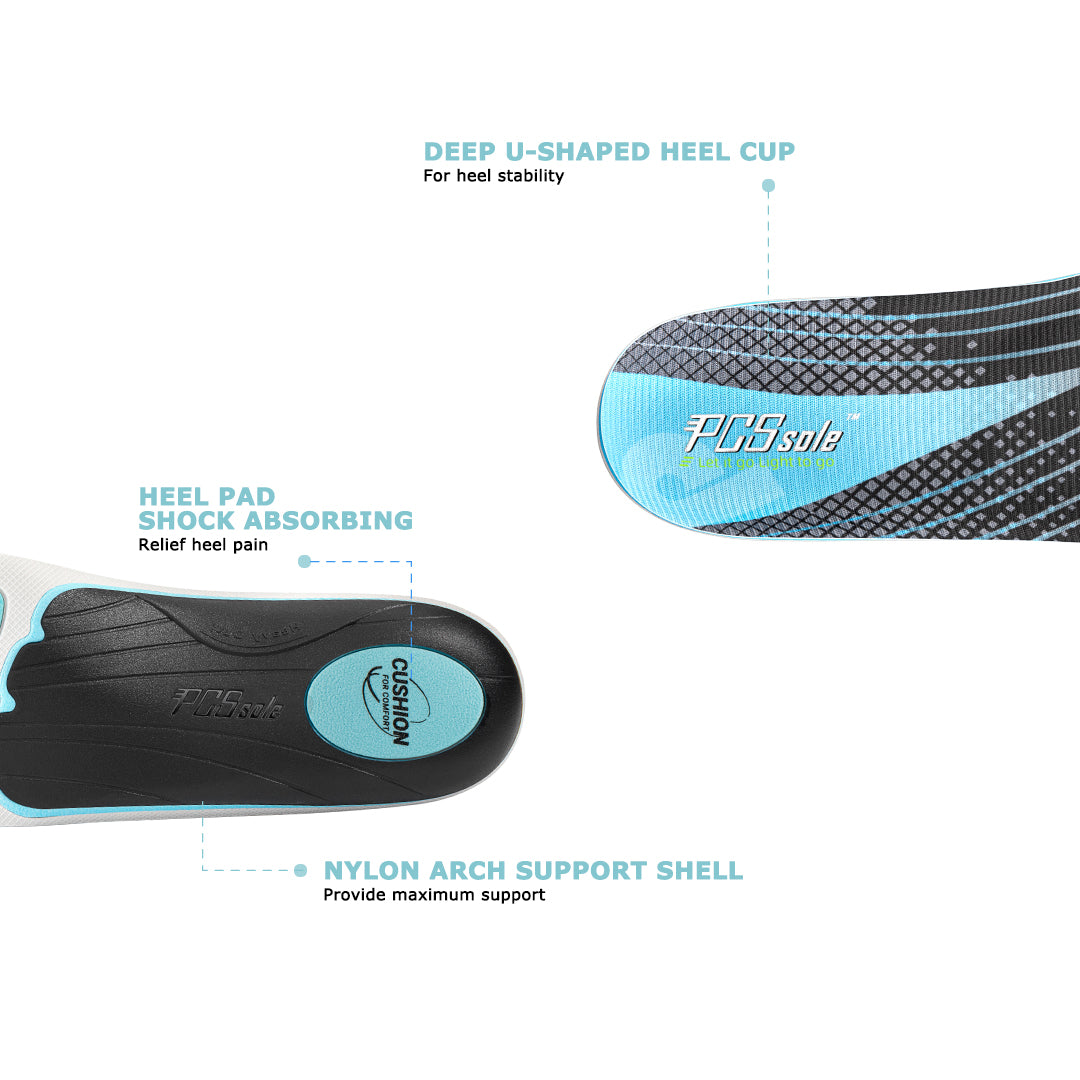
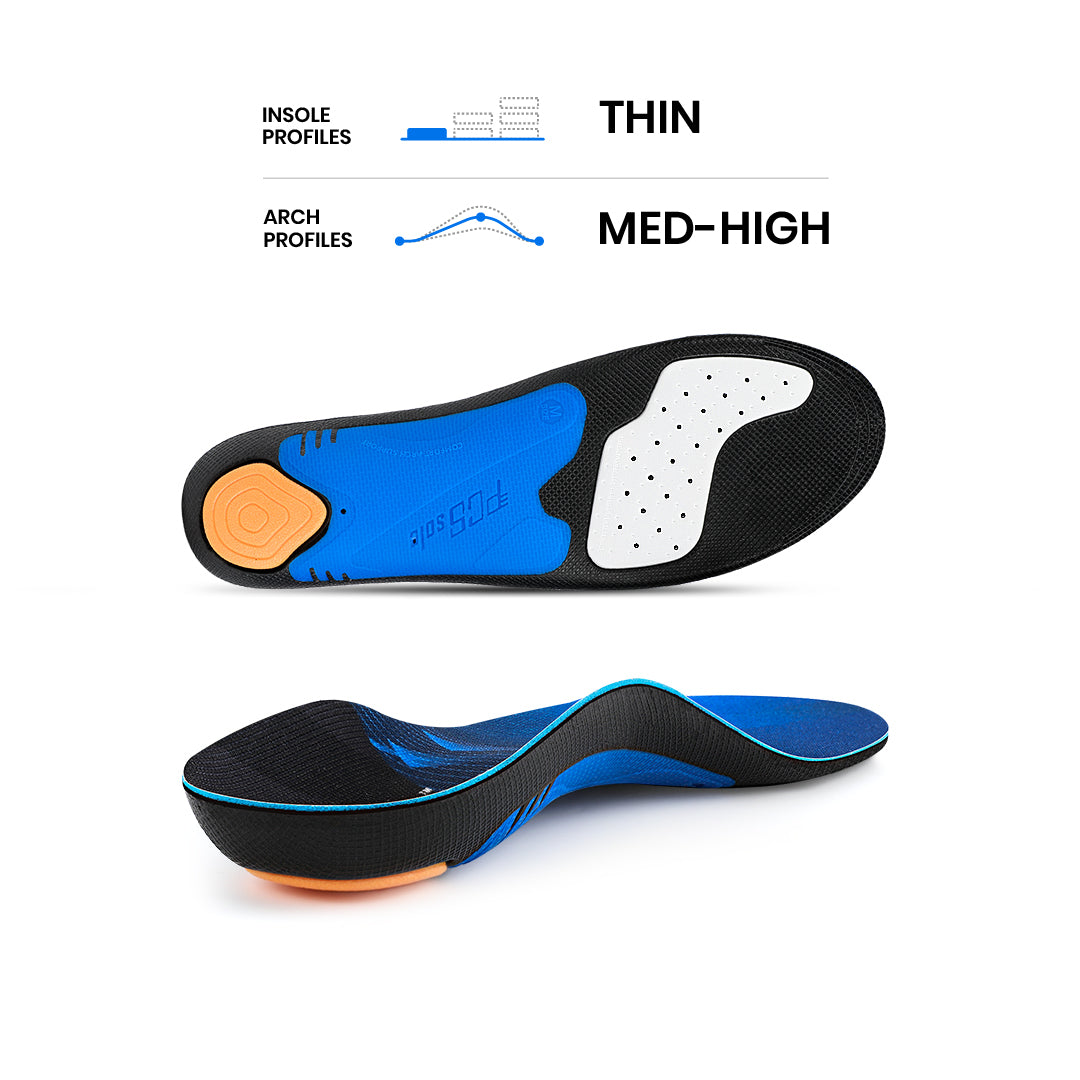
Now, a vital yet often overlooked aspect of peripheral neuropathy management: orthotics and shoe insoles. Custom orthotics—molded inserts tailored to your foot's biomechanics—play a transformative role in alleviating symptoms, especially in the lower extremities where neuropathy hits hardest. By redistributing pressure, correcting alignment issues like pronation or supination, and providing cushioning, orthotics reduce strain on damaged nerves, minimizing pain during walking or standing. In diabetic neuropathy, they prevent ulcers by offloading high-pressure areas (e.g., metatarsals), as evidenced by a Diabetes Care study showing 85% fewer foot injuries with regular use.
For sensory loss, orthotic designs with textured surfaces enhance proprioception—your body's position sense—improving balance and cutting fall risk by up to 50%, per Journal of the American Geriatrics Society data. Materials matter: EVA foam for shock absorption, carbon fiber for rigidity in severe cases, or gel inserts for cooling relief. In the clinic, we pair them with biomechanical exams to address root causes like flat feet exacerbating nerve compression. Affordable over-the-counter options (e.g., PCSsole) work for mild cases, but custom ones from podiatrists yield the best results—expect $200-400 initially, lasting 1-2 years.
Evidence abounds: A Foot & Ankle International review of 20 studies found orthotics improved gait speed and reduced pain scores by 60% in neuropathy patients. For hands (less common but real), ergonomic supports mimic this. Integrate with drinks: A morning smoothie followed by orthotic-clad shoes sets you up for pain-free mobility. Consult a specialist—proper fit is key to avoiding blisters that worsen neuropathy.
Ultimately, peripheral neuropathy isn't a life sentence. With informed choices like these drinks, targeted supplements, and supportive tools like orthotics, 75% relief is achievable. Dive into our book for the full blueprint—years of expertise distilled for you. Reclaim your steps, your sleep, your life. What's your go-to drink? Share below.





















Share:
6 Reasons to Wear Arch Support Insoles for Your Shoes
PCSsole Arch Support Flip Flops Now on Sale(New Arrival)