
When you take your first steps in the morning and feel a sharp pain under your heel, it’s natural to wonder what’s behind it. Even if the discomfort fades as the day goes on, it can still be a frustrating way to start the day. You might assume it’s plantar fasciitis, especially if the pain is concentrated in the arch or heel — but wait, could it be a heel spur?
The Basics...
It's easy to mix up the symptoms of heel spurs and plantar fasciitis, but here's the thing: heel spurs aren't typically the source of your heel pain. Instead, plantar fasciitis usually is.
Plantar fasciitis describes an inflammatory condition of the plantar fascia, impacting roughly two million individuals annually. In contrast, a heel spur represents a bony growth, specifically a calcium deposit, that develops on the calcaneus, commonly known as the heel bone.
Some risk factors for developing plantar fasciitis and heel spurs involve having tight calf muscles, being overweight or obese, wearing unsupportive or ill-fitting shoes, possessing either flat feet or high arches, and exhibiting unusual walking patterns.
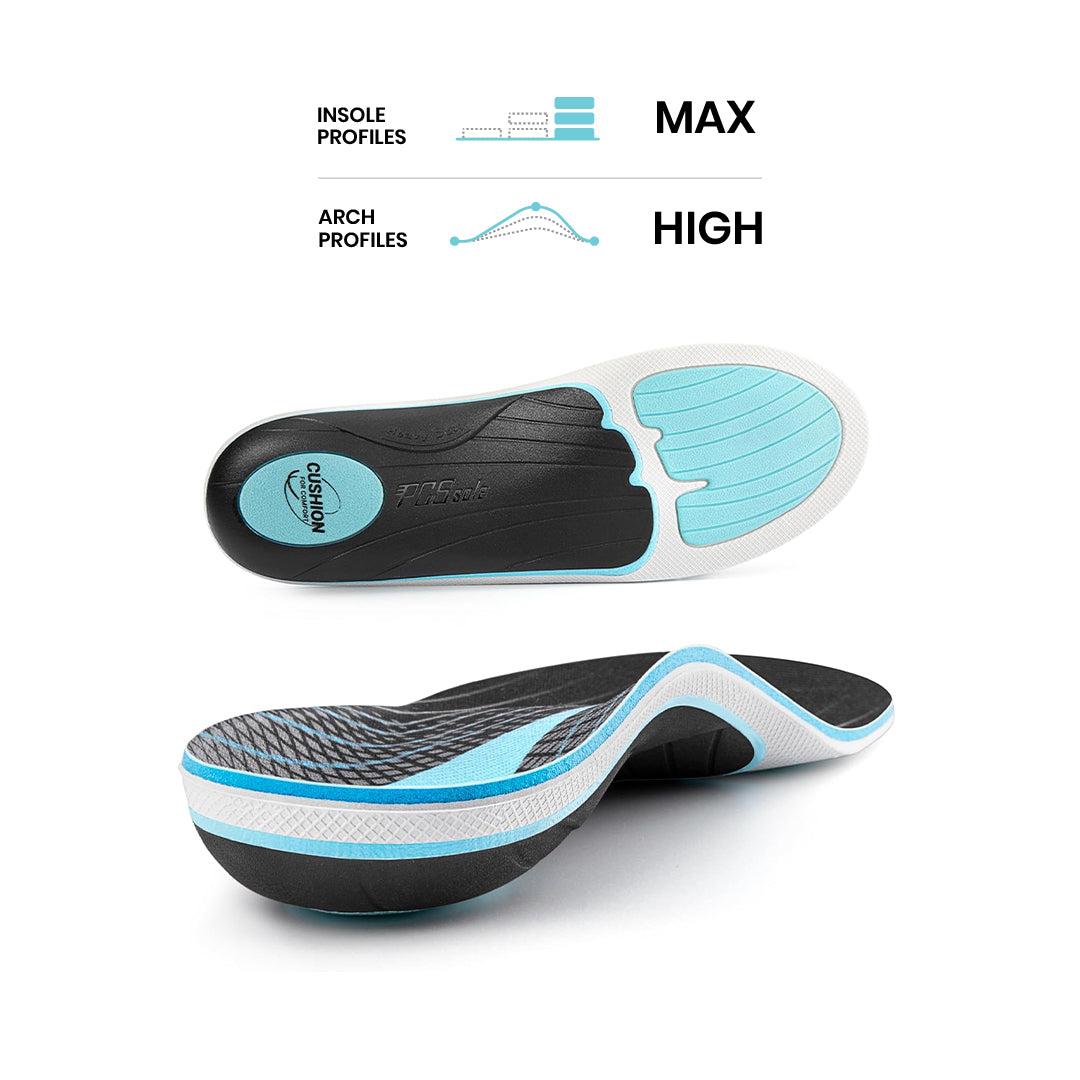
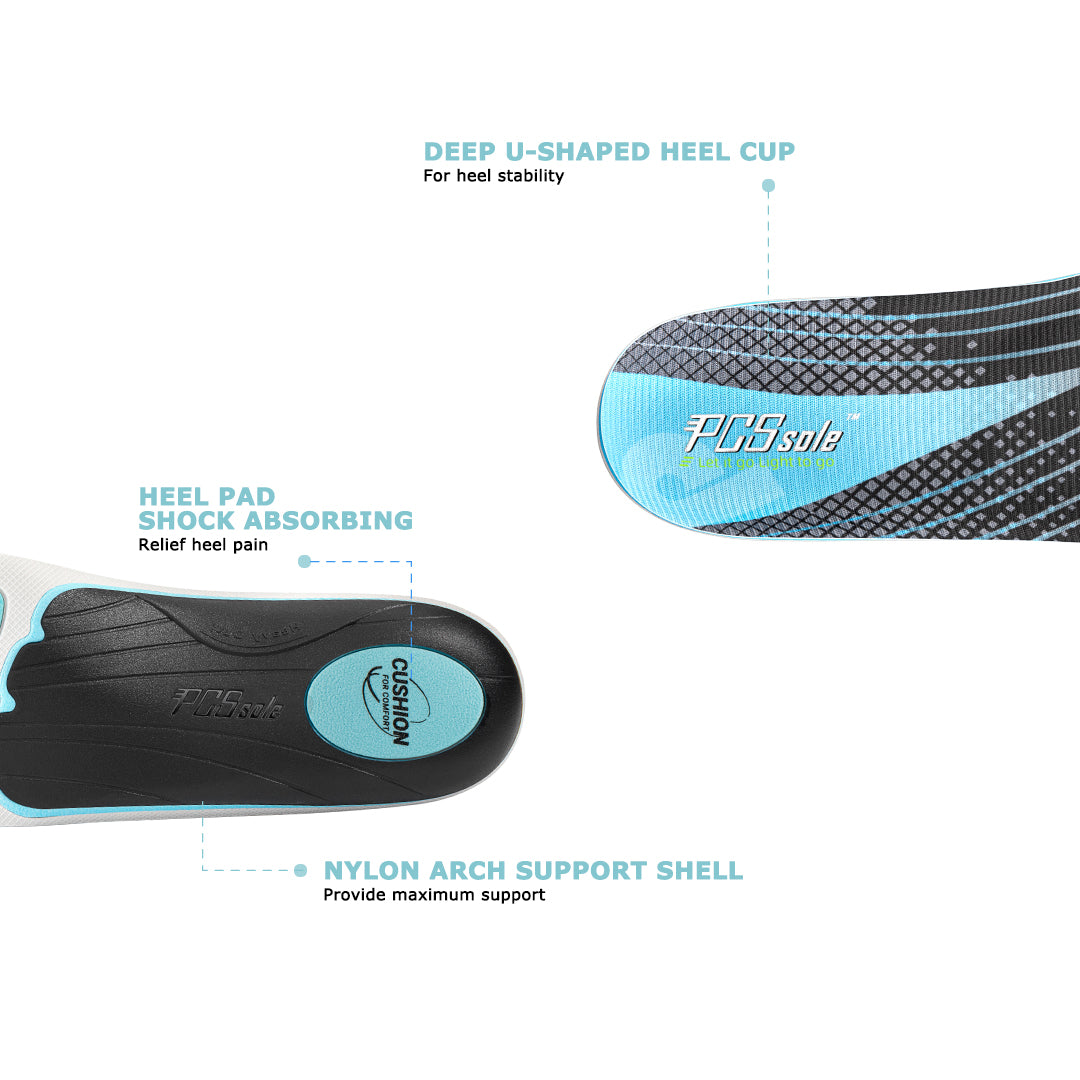
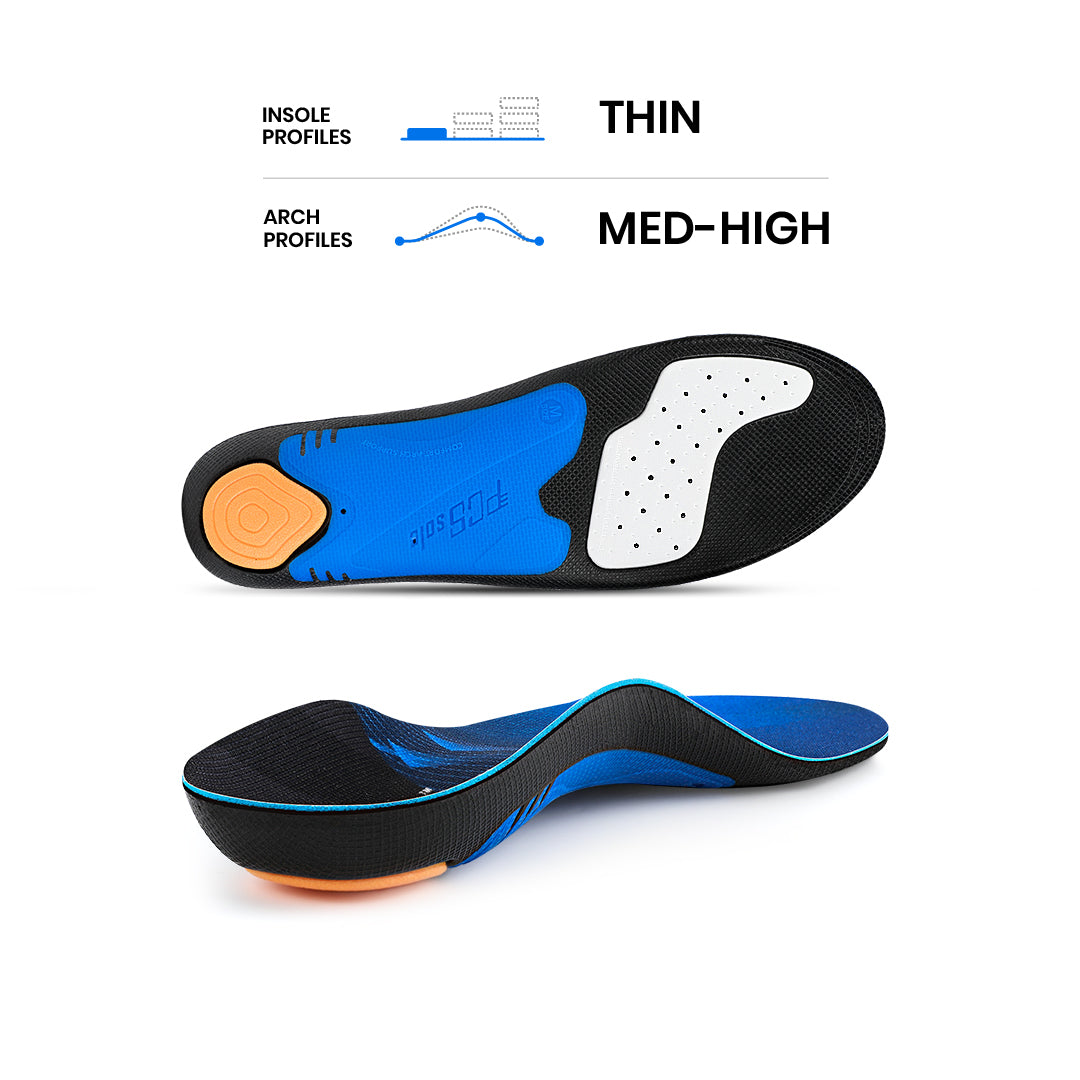
Both heel spurs and plantar fasciitis often respond well to non-surgical approaches, including the use of arch support insoles. For robust, pain-relieving support, we highly recommend Universal Arch Support insoles.

What You Need To Know?
Heel spurs and plantar fasciitis are terms often heard when talking about specific kinds of heel discomfort. Despite being distinct conditions, they can be addressed with the same types of treatment.
What's The Difference Between Heel Spurs and Plantar Fasciitis?
There's a common misunderstanding about the link between plantar fasciitis and heel spurs. Many folks tend to believe that heel spurs frequently trigger heel pain, however that's not the case.
While heel spurs might be associated with discomfort, they're typically not the direct cause of the pain itself, as the Cleveland Clinic points out. Instead, most often when heel pain occurs, plantar fasciitis is the actual culprit.
What is a Heel Spur?
A heel spur, as explained by ScienceDirect, is a type of bone spur, or calcium deposit, that emerges near the rear of the calcaneus (or heel bone), precisely where the plantar fascia connects. These tiny, pointed bony protrusions typically form as a reaction to significant trauma or recurring damage impacting the heel area.
This implies that, in the majority of instances, heel spurs actually develop as a consequence of plantar fasciitis. Should the plantar fascia endure prolonged damage, the body will, over time, form a heel spur to offer the heel supplementary support.
Heel spurs are linked to that familiar sharp, stabbing feeling in the heel, which typically worsens first thing in the morning and fluctuates throughout the day. However, the key distinction is that the heel spur itself is seldom the true source of this discomfort.
Indeed, roughly 10% of the population carries heel spurs, often without even realizing it, yet only about 5% of those with spurs will experience heel pain. The actual cause of pain for most of these individuals, as you might have suspected, is plantar fasciitis.
What is Plantar Fasciitis?
According to Podiatry Today, "plantar fasciitis has reached epidemic proportions, with estimates suggesting that one in six Americans might suffer from the condition." Given its widespread prevalence, comprehending precisely what plantar fasciitis entails is now more crucial than ever.
The plantar fascia is a robust, connective strip of soft tissue, extends from the back of your heel right to the base of your toes. Functioning as a ligament, it links the bones in these regions and is specifically engineered to act as a shock absorber, handling the significant stress your feet regularly endure.
The plantar fascia is incredibly resilient and can handle a lot of force, but excessive pressure can still cause damage or even a tear. When this happens, your body reacts with inflammation, and that inflammation of the plantar fascia is precisely what we call plantar fasciitis.
Plantar fasciitis is typically characterized by a sharp, stabbing sensation beneath the arch and/or along the sole close to the heel. This discomfort often intensifies in the mornings and after extended periods of standing, physical activity, or inactivity. There may also be some redness and swelling in the area.
Sometimes, plantar fasciitis can be mistaken for Achilles tendinitis. As the American Academy of Orthopedic Surgeons explains, "Achilles tendinitis is a frequent ailment that happens when the substantial tendon extending down the back of your lower leg becomes irritated and inflamed."
The Achilles tendon stands as the body's largest and most robust tendon. It connects your calf muscles to the back of your heel, enabling you to rise onto your toes for walking, running, or jumping. However, pushing your training too hard or intensely without sufficient recovery can lead to Achilles tendinitis, resulting in pain localized at the back of your heel or just above it.
How Heel Spurs And Plantar Fasciitis Are Similar
Here's a simple way to distinguish between heel spurs and plantar fasciitis. Lots of folks have heel spurs without ever experiencing plantar fasciitis or any heel pain, yet it's quite uncommon to find someone with plantar fasciitis who doesn't also have a heel spur.
According to one study, roughly 50% of individuals with plantar fasciitis also present with bone spurs. Given that about 1 in 10 people would reveal a heel spur on a foot X-ray anyway, these spurs are only viewed as an incidental—or minor—discovery unless accompanied by actual foot pain.
When a heel spur develops, it typically isn't the direct cause of any foot pain. Instead, that discomfort stems from the underlying foot condition that led to the spur's formation. So, if you have a heel spur and feel pain at the back of your heel, you likely have Achilles tendinitis.
If your pain is located on the bottom of your heel, plantar fasciitis is most probably the culprit. Plenty of people have heel spurs with absolutely no symptoms, and experts are still working to understand how these spurs truly connect to heel pain precisely.
Given that both plantar fasciitis and heel spurs stem from a comparable underlying process, the risk factors linked to them are indeed mutually shared. The subsequent factors elevate the likelihood of developing either condition:
- Tight calf muscles
- Being extremely overweight or obese
- Wearing worn-out, ill-fitting, or unsupportive shoes
- Having flat feet, high arches, or an abnormal walking pattern
- Spending excessive time on your feet
- Participating in sports or activities involving extensive running or jumping
- Increasing physical activity levels too rapidly
It's also crucial to note that while plantar fasciitis and heel spur symptoms appear alike, there's a key differentiator. Plantar fasciitis discomfort can be felt in both the arch and heel, with some patients experiencing it for a period before the sharp heel pain emerges. In the rare instances where a heel spur is the culprit, the stabbing sensation will be precisely localized in the heel itself.

How Do You Treat Heel Spurs And Plantar Fasciitis?
If you're dealing with heel pain, your doctor will likely examine your foot and might suggest an X-ray to confirm what's going on. While plantar fasciitis is the usual suspect for heel pain, it’s important to rule out other causes like Achilles tendinitis, stress fractures, a broken heel, or tarsal tunnel syndrome.
Upon diagnosing either plantar fasciitis or a heel spur, doctors invariably suggest non-surgical treatments as the initial approach, which are typically quite effective. These include rest and ice, a change in footwear, heel cups, insoles, night splints, physical therapy, and cortisone injections:
Rest, Ice, and Pain Relievers – When heel pain flares up, cut back on or stop any activities that worsen it. Try icing the bottom of your foot with a frozen water bottle for about 20 minutes, three to four times daily. Over-the-counter pain relievers like ibuprofen or acetaminophen can also offer temporary relief.
Change Your Footwear – Ensure all your shoes fit properly, aren't worn out, and give your feet ample support. Plus, try to cut back on or completely avoid wearing high heels.
Heel Cups - These plastic, gel or silicone pieces are inserted into just about any pair of shoes. They tackle foot pain by gently elevating the heel, which lessens tension on the Achilles tendon and subsequently eases pressure on the plantar fascia. These cups also offer shock absorption for the heel, further reducing stress on the plantar fascia.
Arch Support Insoles – By offering extra support for your arches, these can significantly lessen the pressure placed on your plantar fascia. Consistently wearing insoles will not only help relieve existing heel pain from plantar fasciitis but also aid in preventing its recurrence.
Night Splints - Designed to treat plantar fasciitis-related heel pain throughout the night. They gently hold your foot and toes in a flexed position, keeping your calf muscles, Achilles tendon, and plantar fascia subtly stretched. Available as boot-style casts, sleep supports, or sock-style options, these provide a straightforward and effective method for easing morning heel pain.
Physical Therapy – stands as a highly common treatment for heel pain. Sessions typically involve comprehensive stretching of both the calves and plantar fascia, alongside manual—or hands-on—techniques performed directly by the therapist.
Cortisone Injections – If these other treatments don't bring down your pain levels, your doctor might recommend an injection of a steroid hormone called cortisone to give you some extra relief.
For people whose pain doesn’t improve after 6-12 months of trying these nonsurgical treatments, surgery is an option.
With such a variety of treatment choices available, it can feel tough to know where to begin. But taking control of your heel pain by finding what works best for you can lead to greater mobility and freedom as your discomfort steadily disappears.





















Share:
Electrolytes and Athletic Performance: Enhancing Endurance for Pros and Amateurs
How to Stretch Achilles Tendon and Loosen a Tight Achilles Tendon