
If you’ve ever experienced a sharp, burning pain in the ball of your foot, felt like you’re walking on a marble, or found yourself constantly taking off your shoes to check for bunched-up socks, you might be struggling with a Morton's neuroma. For years, conventional wisdom has pointed the finger at the usual suspects: high heels, narrow shoes, and high-impact activities.
But here's the truth: everything you think you know about Morton's neuroma could be wrong. Contrary to popular belief, it's not primarily caused by your shoes, daily activities, or even weight gain—though these can certainly make it worse. The real root lies in the intricate mechanics of your foot's structure, specifically the collapse of the transverse arch.
What is Morton's Neuroma?
Morton's neuroma, also known as intermetatarsal neuroma, is a painful condition affecting the ball of the foot. It was first described in 1876 by Dr. Thomas George Morton, a pioneering surgeon who identified it as a benign tumor of the nerve. Despite the term "tumor," it's not cancerous—it's essentially a thickened, scarred nerve tissue resulting from chronic irritation and inflammation.
Morton's neuroma is a neuropathy that usually starts between the third and fourth metatarsals and causes pain that radiates out.
Historically, Morton's neuroma has been associated with external pressures; however, modern holistic approaches, such as those from podiatrists specializing in foot mechanics, reveal a more complex story. It's not just about what's happening on the surface; it's about how your foot's internal architecture fails under stress.
According to experts, Morton's neuroma affects more women than men, possibly due to footwear choices like high heels, but as we'll explore, that's only part of the picture. If you're experiencing foot pain and suspect Morton's neuroma, understanding its definition is the first step toward empowerment.
Common Misconceptions About Morton's Neuroma Causes
When you search online for "Morton's neuroma causes," you'll find a flood of information blaming external factors. Doctors and websites often point to shoes, activities, and lifestyle as the primary culprits. Let's break down these myths:
Myth 1: Shoes Are the Main Cause of Morton's Neuroma
High heels and narrow-toed shoes are frequently vilified for causing Morton's neuroma. The logic seems sound: high heels shift weight to the ball of the foot, increasing pressure, while narrow toe boxes squeeze the toes together, compressing the nerves. Beautiful stilettos or pointed dress shoes can indeed "jam up" the forefoot, leading to irritation.
But while these shoes exacerbate the problem, they're not the root cause. Wearing ill-fitting footwear aggravates an existing mechanical issue in the foot, but it doesn't create Morton's neuroma from scratch. If your foot's structure is stable, even occasional high-heel use might not lead to neuroma formation.
Myth 2: Daily Activities and Sports Trigger Morton's Neuroma
Another common belief is that high-impact activities cause Morton's neuroma. If you're on your feet all day—whether carrying heavy loads, climbing ladders, or engaging in sports like basketball, tennis, or running—the pounding on the forefoot is said to compress nerves and lead to a neuroma.
Sports involving quick stops, jumps, or lateral movements do increase pressure on the ball of the foot, potentially aggravating symptoms. However, these activities are aggravators, not initiators. The real issue starts internally, and without addressing that, even low-impact routines can worsen Morton's neuroma.
Myth 3: Weight Gain Directly Causes Morton's Neuroma
Gaining weight is often cited as a factor because every step multiplies body weight on the forefoot, doubling or tripling the pressure where the neuroma forms. This added load can indeed intensify pain, but it's not the origin. Weight gain amplifies an underlying structural problem, much like how extra cargo strains a weakened bridge.
These misconceptions persist because they focus on visible triggers rather than hidden mechanics. If you've been told your Morton's neuroma is due to shoes or activities, it's time to look deeper.

The Real Cause of Morton's Neuroma: Transverse Arch Collapse
The true culprit behind Morton's neuroma is the collapse of the transverse arch in your foot. Your foot isn't a flat slab; it's a complex system with three arches: the medial (inner) arch, the lateral (outer) arch, and the transverse arch across the ball of the foot.
The transverse arch runs horizontally across the metatarsal heads, acting like a bridge that keeps the forefoot stable and narrow. When this arch collapses—due to genetics, aging, or poor foot mechanics—the metatarsal bones spread apart. This widening stretches the intermetatarsal ligaments, which hold the bones together.
Beneath these ligaments lie the plantar nerves. As the ligaments tighten like a rubber band from the spreading bones, they irritate the nerves underneath. Chronic irritation leads to inflammation, swelling, and scar tissue buildup, forming the neuroma.
Visualizing the Mechanics with a Foot Model
Imagine the metatarsal bones as independent suspension systems, like car tires. The first three metatarsals move together, while the fourth and fifth have their own motion. The most common site for Morton's neuroma is between the third and fourth metatarsals, where excessive motion causes friction.
However, neuromas between the second and third metatarsals are increasingly common, as observed in clinical practice over the past 30 years. The big toe's nerve is spared because of a natural gap between the first and second metatarsals.
When the transverse arch flattens, the entire forefoot widens, tightening ligaments and pinching nerves. This isn't visible externally but explains why Morton's neuroma often coexists with other foot deformities.
Related Foot Conditions That Worsen Morton's Neuroma
Morton's neuroma rarely occurs in isolation. Conditions like bunions (hallux valgus), where the big toe deviates inward, widen the forefoot and strain the transverse arch. Tailor's bunions on the fifth metatarsal do the same on the outer side.
Hammertoes, where toes curl downward like hammers, pull metatarsal heads down, further tightening ligaments and pressuring nerves. If you have bunions, hammertoes, or flat feet, your risk for Morton's neuroma skyrockets because these amplify the arch collapse.
External factors like high heels, sports, or weight gain then pile on, making the irritation worse. High heels elevate the heel, forcing more weight forward and spreading the metatarsals. Sports add impact, and extra weight increases overall pressure. But without the arch collapse, these wouldn't lead to a neuroma.
Understanding this mechanical root is crucial for anyone searching for "Morton's neuroma relief." Treating symptoms without fixing the arch is like patching a leaky roof without repairing the beams—it won't last.

Symptoms of Morton's Neuroma: What Does It Feel Like?
Recognizing Morton's neuroma symptoms early can prevent progression. Patients often describe:
A Marble or Pebble Sensation: It feels like walking on a lump or marble under the ball of the foot, especially between the toes.
Bunched-Up Socks Feeling: Many remove their shoes and socks, convinced something is wadded up inside, only to find nothing.
Numbness and Tingling: Inflamed nerves cause pins-and-needles or numbness in the toes, similar to nerve compression elsewhere.
Toe Cramping: Toes may cramp during walking, at night, or under pressure, due to nerve irritation affecting muscle control.
Clicking Sensation: A subtle click or pop between the toes from the neuroma mass shifting with movement.
Barefoot Pain: Walking barefoot on hard surfaces aggravates pain since the neuroma is close to the skin, lacking cushioning.
Pain worsens with activity and eases with rest or shoe removal. If barefoot walking, especially on tile or wood floors, intensifies discomfort, Morton's neuroma could be the issue.
These symptoms mimic other conditions like stress fractures or arthritis, so professional diagnosis is essential.
Diagnosing Morton's Neuroma: From Exam to Advanced Tests
If you suspect Morton's neuroma, see a podiatrist. Diagnosis starts with:
Physical Examination
The doctor squeezes the forefoot, pressing between the metatarsals (second-third and third-fourth spaces). A positive Mulder's sign—sharp pain or a click—indicates neuroma. Patients often "jump off the table" from the intensity.
Imaging and Tests
X-Rays: Rule out fractures, arthritis, or bone issues in the forefoot.
Ultrasound or MRI: Visualize the neuroma mass, though not always conclusive.
Nerve Conduction Studies (EMG): Assess nerve function from the lower back (L5-S1 roots) down the sciatic nerve to the foot, ensuring no radiculopathy.
Biopsy (Rare): Confirms the benign nerve tumor if needed.
Most cases are diagnosed clinically, but tests exclude mimics like back problems causing referred pain.
How External Factors Aggravate Morton's Neuroma
While not the cause, certain factors worsen Morton's neuroma:
Footwear Choices: Narrow shoes compress toes; high heels shift weight forward.
High-Impact Activities: Running, jumping, or standing jobs increase forefoot stress.
Weight Management: Extra pounds amplify pressure, but losing weight alone won't cure it without arch support.
Barefoot Habits: Hard surfaces directly irritate the neuroma.
Addressing these alongside the arch collapse is key.
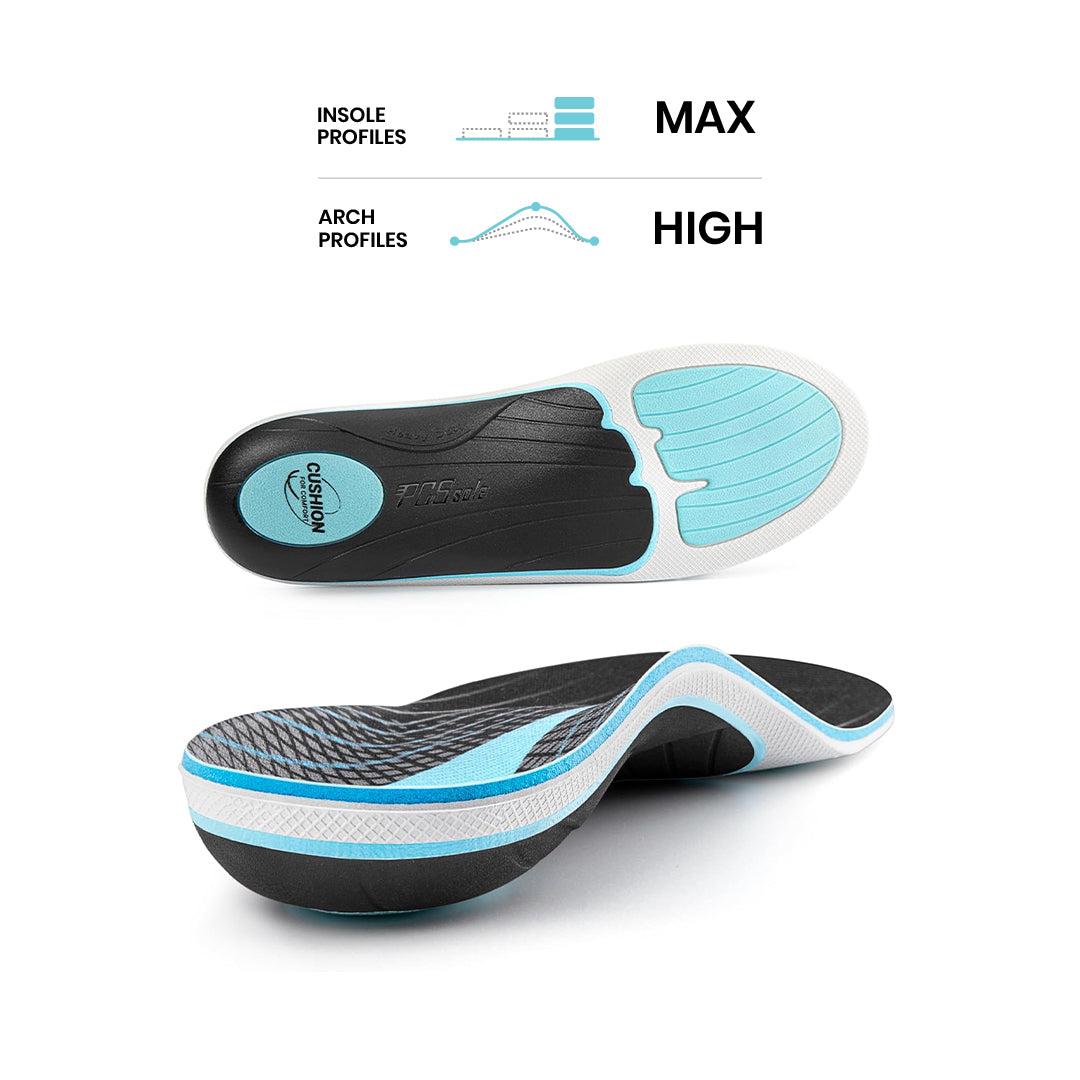
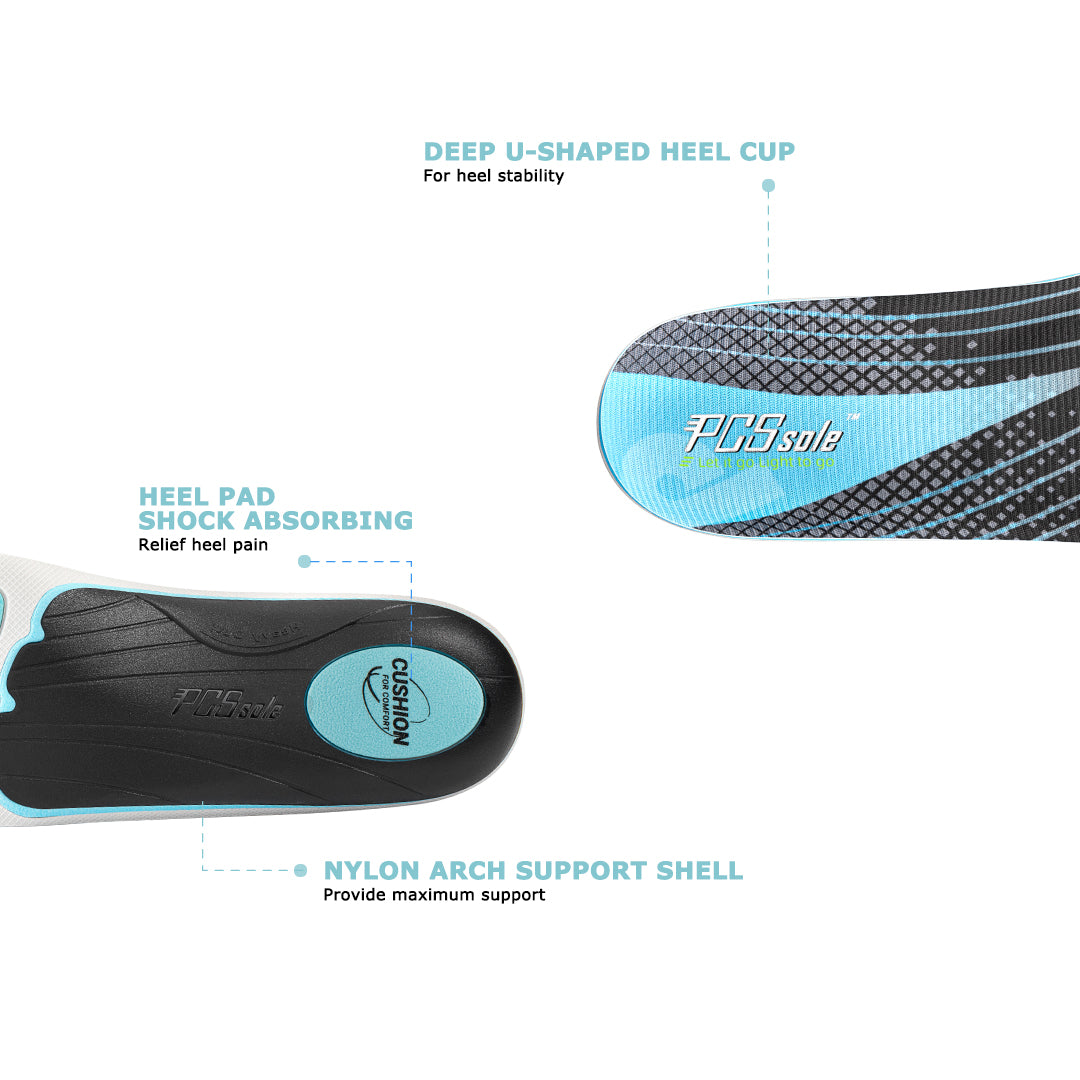
How PCSsole Insoles Can Cure Morton's Neuroma
One of the easy solutions to sort of help some of the pain is to make sure you alleviate have a proper fitting shoe, something that provides enough with length, maybe something with a rounded foot shaped toe box.
The way Altra does.
Another thing is to get an over-the-counter insert that has a metatarsal pad in it.
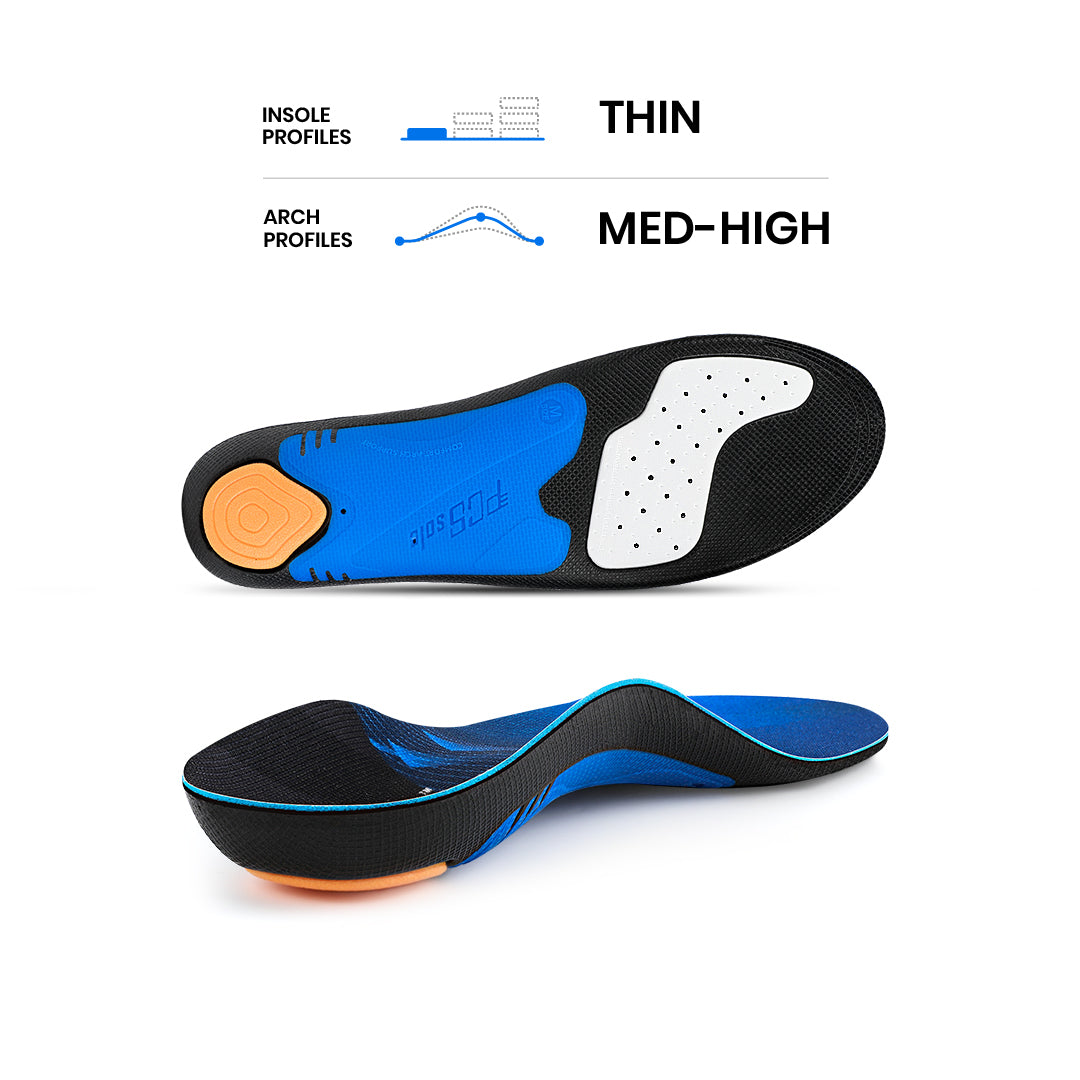
The PCSsole Universal Arch Support insoles have a built-in metatarsal pad that is completely invisible and won’t give you a foreign body sensation on your foot. Most importantly, this metatarsal pad is specially designed to relieve neuropathy or help anyone who puts a lot of pressure on the forefoot (sole).
It sits a little further back than where the actual pain is.
But what this does will help sort of dispel all the different weight issues and help kind of put pressure in different spots, your foot, to alleviate some of the pressure that you're putting on up here. It's a great, helpful fix for Morton's Neuroma.
With a PCSsole over-the-counter insert with the metatarsal pad and a pair of Altras.
For treatment, options range from conservative (padding, injections) to surgical (nerve removal), but holistic approaches emphasize mechanics first.
Living Pain-Free: Empower Yourself Against Morton's Neuroma
Morton's neuroma doesn't have to define your life. By understanding that transverse arch collapse—not just shoes or activities—is the real cause, you can target the source. If symptoms persist, seek a holistic podiatrist who looks beyond surface fixes.
Educate yourself, empower your choices, and encourage others. For more on holistic remedies, explore follow-up resources. Remember, knowledge is your best tool against Morton's neuroma.





















Compartir:
Do You Need a High Arch Insole for Supination?
5 Common Causes of Pain on the Outside of Foot When Walking