
Right now, more than 1 in 3 people in the United States has pre-diabetes, and most have no idea. Your body is designed to warn you about diabetes long before your doctor ever does, so if you have a hunch that might be you, pay attention.
I work hands-on every day with clients trying to reverse their chronic conditions, and I’ve seen how spotting these early warning signs can completely change the outcome. My goal is to help you catch these issues before you get labeled with pre-diabetes or Type 2 diabetes.
Here’s what we’re going to cover:
We’ll walk through 25 of the most common early warning signs or symptoms of diabetes, especially Type 2. We'll go through them rapid-fire with very simple and clear explanations you can actually remember.
We’ll explore what the latest science says about reversing Type 2 diabetes and pre-diabetes completely naturally—without having to follow any crash diets or live in the gym. I’ll also share some of the tips I use with clients to help them manage their blood glucose.
I’ll share the worst mistake I see people making when it comes to blood glucose levels and offer a few tips on how to manage them.
The 25 Most Common Early Warning Signs of Diabetes
These are 25 of the most common early signs and symptoms of diabetes, especially Type 2, and a few of them are probably going to surprise you.
No. 1: Extreme Thirst and Frequent Urination
When your body detects excess sugar in your bloodstream, it works overtime to flush it out. The primary mechanism? Urination. But to produce that extra urine, your kidneys pull water from your tissues, leaving you dehydrated and intensely thirsty. This isn't just a minor annoyance—it's a cycle that can disrupt your sleep and daily routine, with trips to the bathroom happening all day long and even throughout the night. If you're chugging water like it's going out of style but still can't quench that thirst, this is your body's first alarm bell ringing loud and clear.
No. 2: Increased Hunger Even After Eating
You've just finished a meal, yet that gnawing hunger persists. This happens because your cells aren't able to properly absorb glucose from your bloodstream due to emerging insulin resistance. Instead of getting the energy they need, your cells send desperate signals to your brain: "Feed me!" It's like your body is in a state of perpetual starvation at the cellular level, even as your stomach feels full. Over time, this can lead to overeating, which only compounds the blood sugar issues.
No. 3: Unexplained Weight Loss
This one might sound counterintuitive since Type 2 diabetes is often associated with weight gain from insulin resistance. However, if you're suddenly shedding pounds despite no changes in diet or exercise—and especially if you're eating more to combat that constant hunger—it's a major red flag. Your body, overwhelmed by excess sugar it can't utilize, starts breaking down fat and muscle for energy instead. This catabolic process is efficient but destructive, signaling that your metabolism is in distress.
No. 4: Constant Fatigue
If you're dragging through the day, feeling bone-tired no matter how much sleep or coffee you get, and chalking it up to "just getting older," think again. This exhaustion stems from your cells literally starving for fuel. When insulin resistance sets in, glucose can't enter your cells efficiently, and if your body can't access its fat stores either, you're left running on empty. It's a 24/7 wiped-out feeling that saps your motivation and productivity, often mistaken for burnout or aging.
No. 5: Blurred Vision
High blood sugar doesn't just affect your energy levels—it impacts your eyes too. Excess glucose causes fluid shifts in the lenses of your eyes, leading to temporary blurring that can come and go. But if it lingers, it could be an early indicator of something far more serious, like diabetic retinopathy, where delicate blood vessels in the retina begin to damage. Don't dismiss occasional fuzzy vision as eyestrain from screens; it might be your eyes signaling a deeper systemic issue.
No. 6: Slow Healing and Frequent Infections
Notice that a simple cut or scrape is taking weeks to heal, or you're battling recurring urinary tract infections (UTIs), yeast infections, or gum problems? High glucose levels impair your immune system's function, powering it down when you need it most. Imagine your immune cells as the body's vigilant police force—chronically elevated blood sugar is like handing them endless donuts: they become sluggish, distracted, and ineffective at fighting off invaders. This vulnerability turns minor issues into persistent threats.
No. 7: Headaches and Dry Mouth
These aren't always just from skipping your morning coffee or mild dehydration. Blood sugar swings trigger them as your body desperately tries to dilute and expel excess glucose, often by drawing water from saliva production and other tissues. The result? A parched mouth and throbbing headaches that strike frequently. If these symptoms tag-team you often, especially alongside thirst, it's time to investigate beyond the surface causes.
No. 8: Tingling or Burning Sensations in Your Hands and Feet
Often described as "pins and needles" or ants crawling on your skin, this peripheral neuropathy is a direct result of nerve damage from prolonged sugar accumulation. It leads to oxidative stress and inflammation that slowly erodes nerve function, starting in the extremities. This sensation can creep up gradually, but once established, it risks becoming permanent if ignored. Pay close attention—it's not just "poor circulation" from sitting too long.
No. 9: Swollen Ankles and Feet
Excess sugar in your blood doesn't stay benign; it adheres to vessel walls, promoting inflammation and nerve damage that hampers circulation. Fluid then builds up, particularly in the lower body, due to gravity's pull. If your ankles puff up noticeably, especially after standing or at the end of the day, and don't subside with elevation or rest, this edema is a warning that your vascular system is under siege.
No. 10: Cold Feet Resulting from Poor Circulation
Building on the circulation woes from symptom No. 9, elevated blood sugar causes vessels to narrow and stiffen, restricting blood flow to the extremities. Your feet feel perpetually chilly, even in warm environments, and you might notice accompanying signs like shiny skin, numbness, or cramping in your legs. This isn't just a quirky trait—it's a symptom of reduced oxygen and nutrient delivery that can worsen over time.
No. 11: Diabetic Hand Syndrome
If your palms feel unusually tight, waxy, or you struggle to press them flat together without discomfort, this could be limited joint mobility syndrome, a lesser-known but dangerous sign linked to diabetes. It arises from glycation—sugar molecules binding to connective tissues—making them rigid. Early intervention here can prevent broader joint and skin complications.
No. 12: Foot Sores or Ulcers
The deadly duo of numbness (from neuropathy) and poor circulation creates a perfect storm for skin breakdown on the feet. Minor pressure points turn into open sores that heal slowly and are easily irritated. In severe, untreated cases, this progression can lead to amputations—a stark reminder of why foot health checks are non-negotiable for anyone at risk.
No. 13: Dark Skin Patches
Acanthosis nigricans presents as soft, velvety dark folds, typically on the neck, armpits, or groin. This hyperpigmentation is one of the earliest visible markers of insulin resistance, where high insulin levels stimulate skin cell growth. It's subtle at first but a hallmark that your body's sugar-handling system is faltering.
No. 14: Shin Spots
These are brown, scaly patches on your lower legs, sometimes called diabetic dermopathy. They start harmless but signal struggling blood vessels under the assault of chronic high blood sugar. Like rust on metal, they indicate early vascular wear and tear that deserves attention before it spreads.
No. 15: Extremely Dry or Itchy Skin
Particularly on the legs, this dryness goes beyond environmental factors. Excess sugar glycates collagen in the skin, forming advanced glycation end products (AGEs) that disrupt hydration and circulation. That persistent itch isn't random—it's a cry for better blood sugar control to restore skin barrier function.
No. 16: Skin Tags
These small, soft, flesh-colored bumps often cluster on the neck, underarms, or eyelids. While annoying cosmetically, their proliferation is tied to insulin resistance, as excess insulin promotes abnormal skin cell growth. If they're multiplying, view them as tangible evidence of metabolic imbalance.
No. 17: Eruptive Xanthomatosis
Reddish-yellow, waxy bumps resembling pimples erupt on the arms, legs, or buttocks. These lipid-laden lesions are a direct consequence of sky-high triglycerides and blood sugar, screaming insulin resistance and prediabetes. They're not just unsightly—they're a metabolic SOS.
No. 18: Granuloma Annulare
Ring-shaped rashes or bumps encircling areas like wrists or ankles, sometimes itchy, point to immune dysregulation from elevated glucose. Your body's inflammatory response is misfiring, creating these dermatological clues that warrant a deeper health evaluation.
No. 19: Cholesterol Deposits Around Your Eyes (Xanthelasma)
Flat, yellowish plaques near the eyelids aren't just a cosmetic concern—they correlate with high lipid levels and glucose dysregulation. These cholesterol-filled deposits under the skin are an early ocular sign of diabetes, blending vanity with vitality in their warning.
No. 20: Necrobiosis Lipoidica
Shiny, waxy yellowish-brown patches with raised red borders, usually on the shins, can ulcerate if unchecked. This rare but telling condition stems from collagen degeneration due to high sugar, emphasizing the need for prompt vascular and glucose management.
No. 21: Skin Blisters
Painless, fluid-filled bullae that appear spontaneously and heal on their own still signal fragile skin from sugar instability. They're rare but alarming, hinting at broader connective tissue vulnerability that could precede more severe complications.
No. 22: Fungal Infections Like Thrush
Chronic yeast overgrowth—white patches in the mouth (thrush) or red, itchy rashes in moist areas like the groin—thrives on unchecked blood sugar. Yeast is sugar's best friend, so frequent bouts mean your glucose levels are providing an all-you-can-eat buffet for fungi.
No. 23: Staph and Bacterial Skin Infections
Boils, abscesses, or persistent inflamed areas arise because high glucose distracts immune cells, much like overfed police ignoring their duties. These infections linger and recur, underscoring the immunosuppressive effects of hyperglycemia.
No. 24: Red Raised Skin Patches
Erythema-like eruptions that mimic eczema but recur signal early inflammation or brewing infections. Brushing them off as allergies misses the metabolic cue: your skin is the canary in the coal mine for systemic issues.
No. 25: A Protruding Belly
Visceral fat accumulation around your midsection—where your belly precedes your nose when approaching a flat wall—is a classic Type 2 diabetes harbinger. This "apple-shaped" obesity encases organs like the liver and heart in dangerous fat, fueling insulin resistance from the inside out.

Can You Reverse Type 2 Diabetes?
If you've seen a few of these signs and thought to yourself, "Well, that's just getting older," I don't blame you. That's what happened with most of my clients before they got labeled with pre-diabetes or Type 2 diabetes. The good news is you don't have to overhaul your life or live in fear of foods to reverse diabetes and recover your insulin sensitivity; you just need the right course of action.
The real key is not just about taking medications or supplements; it's about calming the three forces that drive high blood sugar:
Insulin Resistance: Insulin is your storage hormone. Insulin resistance happens when you have too much sugar, so your body produces more insulin, and then the cells say, "No more," and they get resistant to insulin bringing them that sugar.
Chronic Inflammation: Inflammation is like rust; it slows things down, causes malfunctions, and ultimately blocks glucose in your bloodstream from being used.
Daily Blood Glucose Spikes: When your glucose is always being spiked, you keep your system overloaded. You're never giving your body a rest.
When you address those three things with the right nutrition, movement, and stress management strategy, your body and your insulin start responding again. This is why so many of my clients can lower their HbA1c, their blood glucose, their fasting insulin, lose weight, and feel more energy than they have in years.

The Biggest Mistake People Make and How to Avoid It
There's one mistake that almost everybody seems to make: they try to fix their blood sugar without actually knowing what's causing the issue. That's like trying to drive when you have the parking brake on. No matter how hard you push, you may start moving, but eventually, you're going to burn out your engine.
Don't just chase lower blood sugar. If you're only focused on numbers without addressing why they're high in the first place, you're going to stay stuck. You want to fix the underlying mechanism, not just the measurement. That means focusing on insulin sensitivity, liver health, and inflammation.
If you're serious about reversing pre-diabetes or Type 2, or regaining your insulin sensitivity, start here:
Eat in This Order: When you have your meals, start with fiber, then have your proteins and fats, and then have your carbs (if you're going to have any at all). Eating your fiber first creates a mesh in your stomach that actually slows glucose absorption, which reduces blood sugar spikes and protects your insulin.
Move After Every Meal: Walk for 10 to 15 minutes or just do 15 to 20 bodyweight squats after every single meal. Muscle is your most metabolically active tissue and is very hungry for sugar, but only if you activate it. Activating the biggest muscles in your body (your legs) can actually lower the post-meal glucose spike by up to 30%.
Follow the "No GPS Rule": This is the number one nutrition rule for protecting your blood sugar. GPS stands for Grains, Potatoes, and Sugar. Think white bread, white rice, juices, sodas, cereals, granola bars, and even regular potatoes.
Hydrate Aggressively: Aim to drink 2 to 3 liters of water a day. This will help flush your system, reduce dehydration from high blood glucose, and support fat metabolism.
The Psychology Hack
Imagine this: anytime you eat food, it's like pulling a lever in your body. Some foods pull it more than others, and that lever releases insulin. If you're dealing with diabetes or pre-diabetes, your goal is to try and reduce the frequency and intensity with which you're pulling that lever.
Remember, your body is going to warn you long before your doctor does. Now you know what to look for, and more importantly, what to do next.
What does Diabetes do to Your Feet?
When left uncontrolled, diabetes can cause several complications, including foot health issues.
Neuropathy: If diabetes is not treated properly, it can cause neuropathy, or nerve damage in the feet called neuropathy. Neuropathy is a loss of feeling heat, cold or pain. The loss of sensation can make it difficult to feel injury, such as burning from hot sand or blisters forming from your shoes. When left untreated, even the smallest of injuries can lead to major complications like serious infection and potentially amputation.
Infections: Diabetes also affects the flow of blood throughout your body. This lack of effective blood circulation makes it harder for a sore or cut to heal. If your foot sustains an injury and there isn’t adequate blood flow to help heal the wound, there is a risk of the tissue developing necrosis, or dying and eventually becoming gangrene. In order to stop the spread of gangrene, the dead tissue needs to be removed completely from the body. In serious cases, amputation is used to remove a toe, foot or portions of the leg with gangrene. With proper care and treatment, this can be prevented.
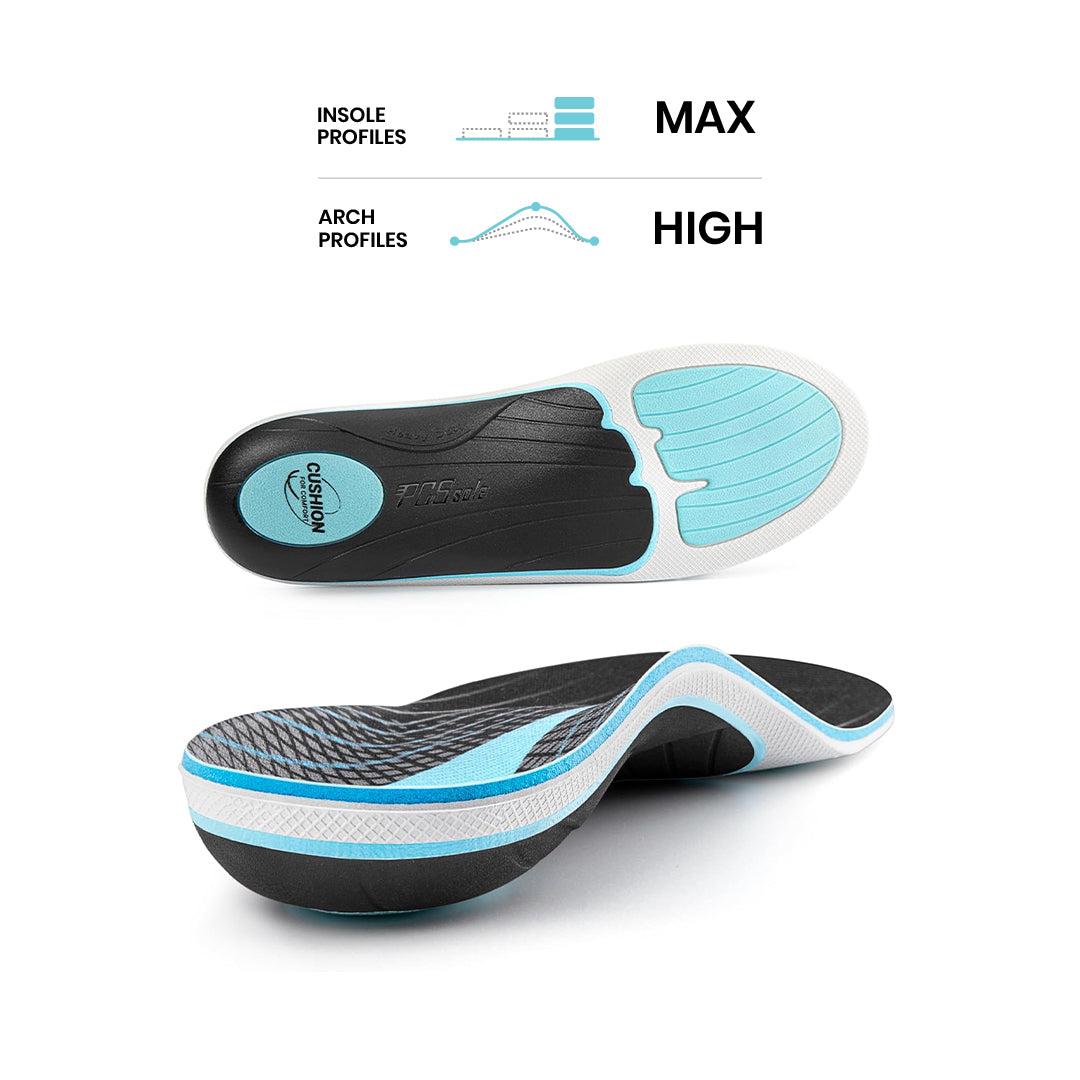
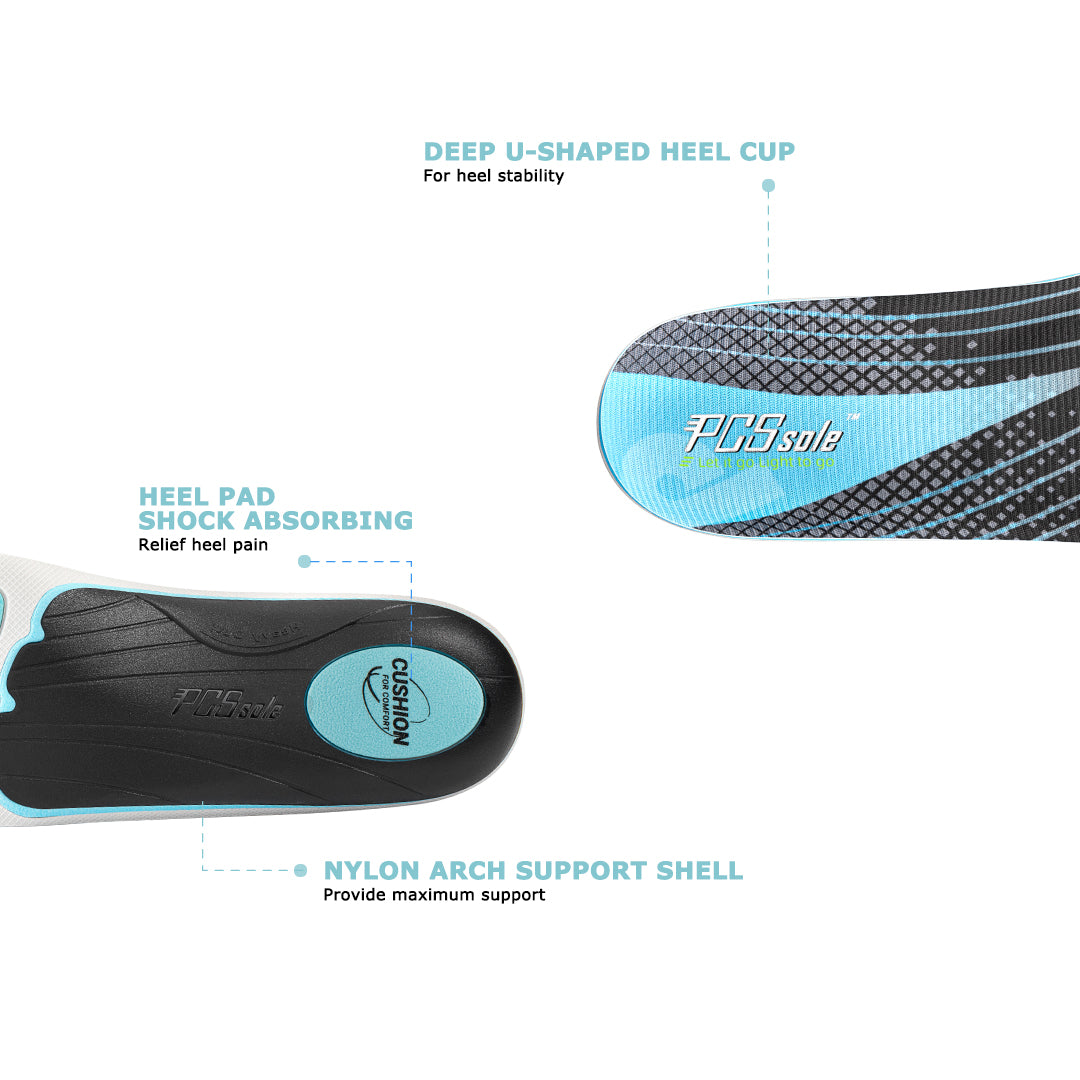
Diabetic Insoles vs. Diabetic Shoes: Making the Choice
The decision between diabetic insoles and diabetic shoes ultimately depends on your individual needs and custom foot insoles preferences.
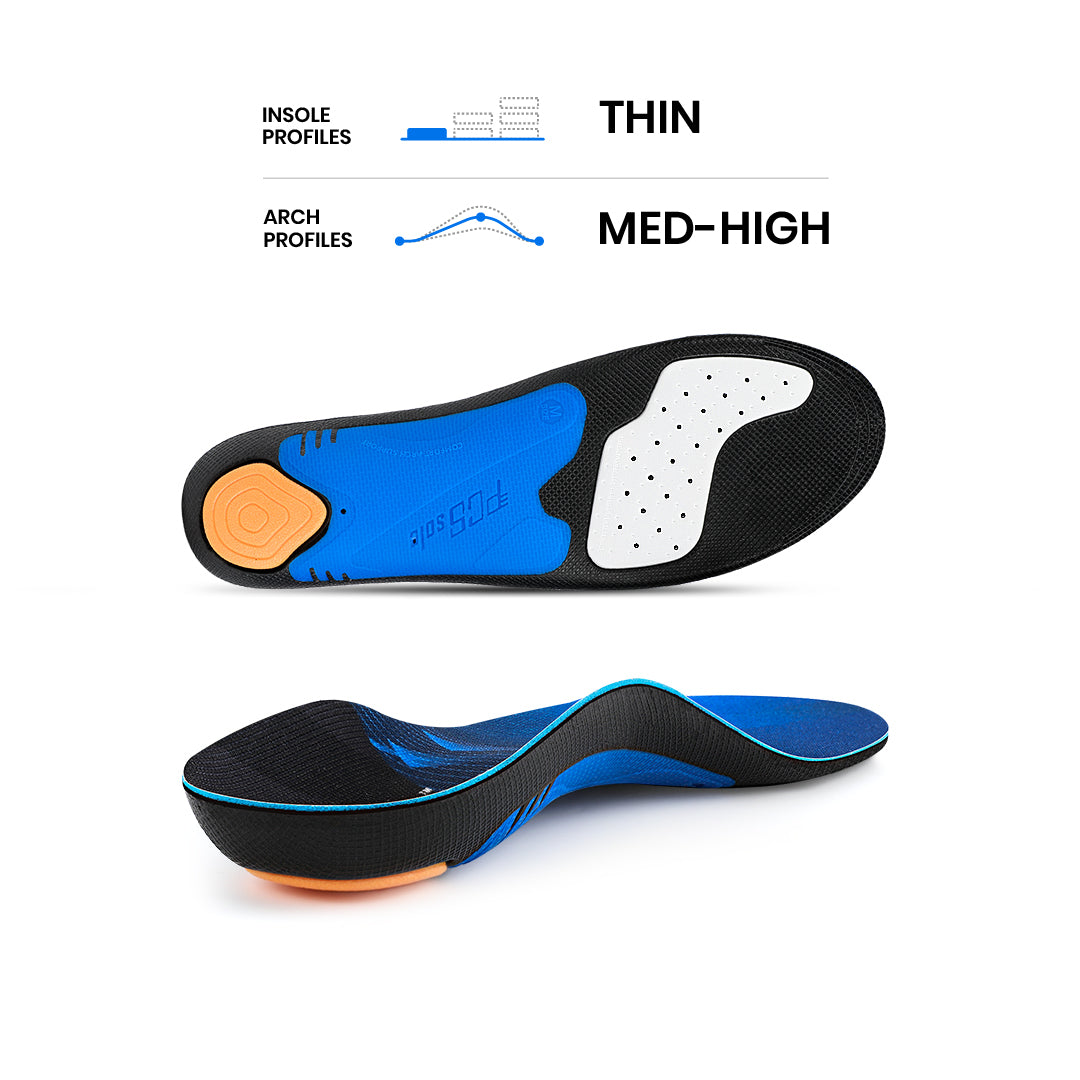
Diabetic Insoles: If you have well-fitting and supportive shoes that you love to wear, adding diabetic insoles could be an excellent option. These insoles can enhance the comfort and protective features of your existing footwear, especially if you’re looking for targeted support in specific areas.
Diabetic Shoes: If you’re seeking an all-in-one solution that doesn’t require inserting specialized insoles into your shoes, diabetic shoes are a practical choice. They provide comprehensive foot support, cushioning, and protection, minimizing the risk of foot problems and complications.
In the realm of diabetic foot care, both diabetic insoles and diabetic shoes play integral roles. The decision between the two depends on your lifestyle, existing footwear, and personal preferences. Remember, prioritizing foot health is essential for individuals with diabetes, and choosing the right option – be it diabetic insoles or diabetic shoes – can significantly reduce the risk of complications, ensuring that you continue to move comfortably on your journey towards overall well-being. Always consult with your healthcare provider or a podiatrist before making a decision, as they can provide personalized guidance tailored to your specific needs.





















Compartir:
Best Ball of Foot Pain Relief 2026: Metatarsalgia Treatment In ONE Step
The Benefits of Jogging: The Secret to Longer Life?